RJPS Vol No: 15 Issue No: 4 eISSN: pISSN:2249-2208
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Visveswarspura Institute of Pharmaceutical Sciences, Bangalore, Karnataka, India
2Visveswarspura Institute of Pharmaceutical Sciences, Bangalore, Karnataka, India
3Visveswarspura Institute of Pharmaceutical Sciences, Bangalore, Karnataka, India
4Sabareesh Subramanian A, Visveswarspura Institute of Pharmaceutical Sciences, BSK 2nd Stage, Bangalore, Karnataka, India.
*Corresponding Author:
Sabareesh Subramanian A, Visveswarspura Institute of Pharmaceutical Sciences, BSK 2nd Stage, Bangalore, Karnataka, India., Email: sabareeshsubramanian@gmail.com
Abstract
Background: Post-operative pain is experienced by the majority of patients and can be managed using a single analgesic agent or through multimodal analgesia.
Objective: To evaluate the prescription patterns of analgesics and assess pain management among post-operative patients.
Method: This was a prospective observational study conducted on 400 patients over a six months period. Data collected included patient demographics (age, gender), chief complaints, diagnosis, laboratory test results, and details of the drugs prescribed, such as generic/brand name, dose, frequency, route of administration, and duration of treatment. Assessment of pain was done using the Numerical Rating Scale.
Result: Out of 400 patients, 243 were male (60.75%) and 167 were female (39.25%). The largest proportion of subjects belonged to the 46-60 years age group (33.75%). Majority of subjects reported mild pain (52.75%). Most drugs were prescribed by brand name (88.1%). Intravenous administration was the most common route (97.14%). Tramadol was the frequently prescribed monotherapy on the day of surgery (16.25%), whereas paracetamol was the most commonly prescribed monotherapy on postoperative days 1 (42.96%), 2 (61.61%), and 3 (69.37%). The combination of tramadol and paracetamol was the most commonly prescribed combination therapy on postoperative day 0 (40.25%), day 1 (26.04%), day 2 (15.16%), and day 3 (7.5%).
Conclusion: This study highlights the need to curb irrational prescribing to reduce morbidity and ease the public health burden. Promoting the judicious use of all medications, including analgesics, can lower costs, limit adverse effects, and improve care delivery.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
The International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory and emotional experience associated to real or potential tissue injury, or described in terms of such injury.1
Pain is a subjective experience that cannot be objectively defined or quantified satisfactorily; therefore, its management should be guided according to the patient’s response and by selecting the most appropriate analgesic.2,3 Selection of appropriate dose, route, technique of administration helps minimize adverse effects, and analgesic therapy should be individualized for each patient.3
Analgesics are defined as drugs that relieve pain without blocking nerve impulse conduction or markedly altering sensory function.4
Post-operative pain is experienced by the majority of patients, and its severity depends on the nature and site of the surgical injury. Severity of pain can vary widely, even among patients undergoing the same procedure.5 Effective pain management is essential for optimal patient care after a surgical intervention. Ineffective management may lead to prolonged hospital stays and increased morbidity.6 Pain management practices are followed in tertiary care hospitals, which handle a high volume of patients. Complications that can contribute to acute post-operative pain include embolization, delayed healing, and delayed recovery. If inadequately treated, post-operative pain may progress to chronic pain, which can impair quality of life. Therefore, effective pain management is essential in post-operative patients.7
An appropriate assessment tool is essential for effective acute post-operative pain management. In this study, the Numerical Rating Scale (NRS) was used, consisting of a 1-10 scoring system in which 1 indicates no pain and 10 represents the worst possible pain imaginable. The rating assigned to the patient’s pain depends on the observer.
Major disadvantages in pain management include insufficient knowledge regarding analgesic use, incomplete documentation of medications administered for pain, and the infrequent use of standardized pain-assessment methods.8 These issues can be addressed by gaining strong knowledge regarding the adverse effects of the prescribed analgesics and by incorporation of appropriate assessment tools.7
Post-operative pain can be managed with a single analgesic or a combination of two or more analgesics, a strategy known as multimodal analgesia.5
Opioids act as agonists on central and peripheral opioid receptors and may be administered through different routes like rectal, sublingual, transdermal, subcutaneous, intramuscular or intravenous. Intravenous infusion provides a more consistent blood levels. Opioids do not exhibit a ceiling effect.
NSAIDs are used widely to treat pain and inflammation. Although they are less potent than narcotics, they lack many of the side effects associated with opiates and therefore can serve as opiate-sparing agents. The availability of more potent NSAIDs like diclofenac and ketorolac has contributed to their increased use in postoperative pain management. However, side effects such as peptic ulcer disease, gastrointestinal haemorrhage, renal dysfunction, altered liver function, and platelet dysfunction may limit their use in post-operative patients.9
Combining analgesics that act through different mechanisms and have distinct pharmacokinetic profiles pro-vides a broader spectrum of pain relief and reduces the side effects associated with higher doses of multiple, single drug analgesic interventions. Numerous studies indicate that multimodal analgesia is an accepted approach for post-operative pain treatment in Asian patients.10
With this in view, the present study was conducted to assess pain management, evaluate the prescription patterns of analgesics in post-operative patients, and create awareness regarding analgesic use among hospitalized patients at KIMS Hospital and Research Centre, Bangalore.
Materials and Methods
A prospective observational study was conducted for a period of six months (30/4/22 – 30/10/22). A total of 400 inpatients from the General Surgery Department at KIMS Hospital and Research Centre, Bangalore, India, who met the study criteria, were included. Participants were selected based on inclusion and exclusion criteria after obtaining ethical clearance from the KIMS institutional ethical committee (KIMS/IEC/D008/P/2022). Data were collected only after obtaining informed consent from each patient. Patient information was gathered from the in-patient records of post-operative patients in the General Surgery Department and included sociodemographic details such as age and gender, detailed medical history including comorbidities, medications, and risk factors, along with clinical examination and pertinent investigations, and information on the drugs prescribed, such as brand and/or generic name, dose, dosing frequency, route of administration, and duration of treatment.
The procedure was as follows:
(a) Patient enrolment
(b) Documentation of data using a self-designed data collection form
(c) Determination of prescription patterns
(d) Pain assessment using Numerical Rating Scale
(e) Data entry in MS Excel and analyis using SPSS version 28.
Study Criteria
Inclusion criteria
• All post-operative cases in the General Surgery Department
• Patients willing to provide consent
Exclusion criteria
• Patients who consumed alternative medicines such as herbal, Ayurvedic, or Homeopathic treatments
• Unconscious patients with diminished chances of survival and unstable vital signs
Results
Demographic Details
In the current study, 400 patients were enrolled, of whom 243 were men (60.75%) and 157 were women (39.25%). Regarding age distribution, four subjects (1%) were younger than 18 years, 75 patients (18.75%) were between 18 and 30 years, 109 patients (27.25%) were between 31 and 45 years, 135 subjects (33.75%) were between 46 and 60 years, 60 patients (15%) were between 61 and 75 years, and 17 patients (4.25%) were older than 75 years.
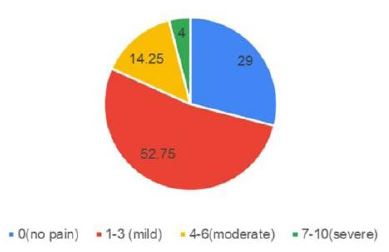
The image shows the distribution of pain levels using the Numerical Rating Scale (NRS). Most individuals (52.75%) reported mild pain (score 1-3), followed by 29% with no pain (score 0). Moderate pain (score 4-6) was seen in 14.25%, and only 4% experienced severe pain (score 7-10). This indicates mild pain is the most common category (Figure 1).
The image shows the distribution of drugs based on brand and generic names. It indicates that 88.11% of drugs are brand names, while only 11.89% are generic names. This suggests a strong preference or dominance of brand-name drugs over generic alternatives in the dataset (Figure 2).
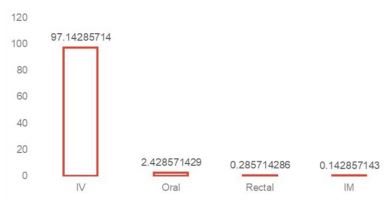
The image illustrates the distribution of drug administration routes. It shows that Intravenous (IV) administration dominates with 97.14%, while oral accounts for 2.43%, and rectal (0.29%) and intramuscular (IM) (0.14%) are minimal. This indicates IV is the most commonly used route by a significant margin (Figure 3).
The table shows the distribution of analgesics prescribed over four days. Paracetamol (PCT) was the most frequently used drug, especially on Day 1 (42.9%), Day 2 (61.6%), and Day 3 (69.3%). Among combination therapies, Tramadol + Paracetamol (TRA+PCT) was most common, with 40.25% on Day 0 and 26.04% on Day 1. This indicates a strong preference for paracetamol, both alone and in combination (Table 1).
Discussion
Of the 400 patients included in the study, 157 (39.25%) were female and 243 (60.75%) were male. This distribution was comparable to the findings of Farhad Marghoubi et al., who also reported a higher proportion of male patients (104, 71%) compared to female patients (43, 29%).11
In this study, four participants (1%) were under the age of 18, 75 participants (18.75%) were between 18 and 30 years, 109 subjects (27.25%) were between 31 and 45 years, and 135 subjects (33.75%) were between 46 and 60 years. This could be due to the greater involvement of these age groups in socioeconomic activities that contribute to stress, as well as an age-related increase in disease susceptibility that often necessitates surgical interventions.12 Additionally, 60 participants (15%) were between 61 and 75 years of age, 17 subjects (4.25%) were older than 75 years. This distribution contrasts with the findings of Farhad Marhoubi et al., in which the majority of patients were between 18 and 30 years of age.11
Pain was evaluated using the Numerical Rating Scale. A total of 116 patients (29%) reported no pain (score of 0).
Mild pain was reported by 211 patients (52.75%), moderate pain by 57 patients (14.25%), and severe pain by 16 patients (4%), corresponding to scores 7-10.
Although the National List of Essential Medicines (NLEM) in India promotes prescribing medications by their generic name, in our study, 615 drugs (88.1%) were prescribed by brand name, while only 83 drugs (11.89%) were prescribed by generic name. These findings are similar to those reported by Farhad Marghoubi et al. (87% prescribed by trade name and 13% by generic name) and Chandrakantha et al. (88% by brand name and 12% by generic name).11,13 However, this contrasts with the study by Vidisha Vivek Parulekar et al., in which 79.56% of drugs were prescribed by generic name. According to WHO standards, 100% of drugs should be prescribed by generic name. Prescribing by generic name reduces cost and minimizes confusion during prescribing, thereby promoting more rational use of drugs.12
A total of 680 drugs (97.14%) were administered intravenously, 17 drugs (2.42%) were administered orally, two drugs (0.28%) were administered rectally, and only one drug (0.14%) was administered intramuscularly. These findings are comparable to those of Farhad Marghoubi et al., who reported that 47 patients (17%) received oral therapy, while 233 patients (83%) received IV therapy.11
Of the 400 subjects, 161 received monotherapy and the remaining 239 received combination therapy. On the day of surgery, all patients received analgesics via the parenteral route. Among the 400 subjects, tramadol was administered to 65 subjects (16.25%). This finding contrasts with studies by Chandrakantha T et al., and Shivaleela Barawade et al., in which diclofenac was the most commonly prescribed analgesic.13,14 Tramadol has minimal side effects such as limited cardiorespiratory depression and low addiction potential, which may contribute to better patient adherence. It is also widely available, cheaper, and offered in an oral formulation. Diclofenac was administered to 35 subjects (8.75%), paracetamol to 60 subjects (15%), and nefopam to one subject (0.25%).
A total of 161 subjects (40.25%) received the combina-tion therapy of tramadol and paracetamol. This contrasts with the findings of Vinoothna Bavireddy et al., in which aceclofenac + paracetamol was the most commonly prescribed combination. In the present study, 16 subjects (4%) received tramadol + diclofenac, 38 subjects (9.5%) received paracetamol + diclofenac, two subjects (0.5%) received fentanyl + paracetamol, 11 subjects (2.75%) received tramadol + paracetamol + diclofenac, and three subjects (0.75%) received diclofenac + paracetamol + aceclofenac. Another three subjects (0.75%) received ibuprofen + paracetamol + tramadol. Additionally, aceclofenac + paracetamol, nefopam + diclofenac, tramadol + paracetamol + aceclofenac, fentanyl + paracetamol + diclofenac, and ibuprofen + tramadol + paracetamol + diclofenac were administered to one subject each (0.25%).
A total of 384 subjects received analgesics on the first postoperative day. Among them, tramadol was administered to 35 subjects (9.11%), and paracetamol was administered to 165 subjects (42.96%), although paracetamol has a greater antipyretic effect than analgesic effect due to selective COX-3 inhibition.14 Diclofenac was given to 37 subjects (9.63%), 100 subjects (26.04%) received tramadol + paracetamol, four subjects (1.04%) received paracetamol + aceclofenac, seven subjects (1.82%) received tramadol + diclofenac, diclofenac + paracetamol was given to 20 subjects (5.208%), tramadol + paracetamol + diclofenac was given to six subjects (1.562%), ibuprofen + paracetamol + tramadol to five subjects (1.3%). Additionally, paracetamol + diclofenac + aceclofenac, ibuprofen + paracetamol + tramadol + diclofenac, fentanyl + paracetamol, ibuprofen + paracetamol, and tramadol + aceclofenac + paracetamol were administered to one subject each (0.26%).
Among the 400 subjects, 310 subjects received analgesics on the second postoperative day. Tramadol was administered to 17 subjects (5.48%), paracetamol to 191 subjects (61.61%), and diclofenac to 23 subjects (7.41%). Combination therapy of tramadol + paracetamol was administered to 47 subjects (15.16%), paracetamol + diclofenac to 15 subjects (4.83%), paracetamol + aceclofenac to five subjects (1.61%), diclofenac + paracetamol + aceclofenac to two subjects (0.64%), ibuprofen + paracetamol + tramadol to three subjects (0.96%), ibuprofen + paracetamol to three subjects (0.96%). Additionally, paracetamol + diclofenac + tramadol, ibuprofen + paracetamol + tramadol + diclofenac, aceclofenac + paracetamol + tramadol, diclofenac + tramadol were administered to one subject each (0.32%).
Among the 400 subjects, 160 subjects received analgesics on the third postoperative day. Five subjects (3.12%) received tramadol, 111 subjects (69.37%) received paracetamol, 18 subjects (11.25%) received diclofenac. Combination therapy of diclofenac + paracetamol was administered to three subjects (1.87%), 12 subjects (7.5%) received tramadol + paracetamol, three subjects (1.87%) received ibuprofen + paracetamol. Additionally, diclofenac + tramadol, ibuprofen + paracetamol + tramadol, aceclofenac + paracetamol + diclofenac, and tramadol + paracetamol + aceclofenac were administered to one subject each (0.625%). This finding was comparable to the study conducted by Farhad Marghoubi et al., in which tramadol was prescribed for 65 patients (44.2%).11
Conclusion
This prospective observational study analyzed the distribution of analgesics, their combinations, routes of administration, and pain. Most participants were male, with majority aged between 46 and 60 years. Most drugs were prescribed by brand names; these may be replaced by generics to improve rational use. Intravenous administration was the most commonly used route, and all analgesics were given in this manner on the day of surgery. Pain was assessed using the Numerical Rating Scale. Pain was the most frequently reported post operative symptom. While tramadol was commonly used on the day of surgery for severe pain, paracetamol was the most frequently prescribed analgesic on the first, second, and third postoperative days. This pattern suggests an initial use of opioid analgesia followed by transition to NSAIDs, demonstrating effective evidence-based post operative pain management. Tramadol + paracetamol was the most popular combination across all three postoperative days. The findings of this study emphasize the importance of minimizing irrational prescribing to reduce morbidity and lessen public health care burden. Ensuring reasonable use of all medications, including analgesics, can reduce costs, minimize adverse effects, and improve health care delivery. Establishing a hospital formulary and ensuring strict adherence by prescribers may further enhance rational drug use. Health care quality can be improved by implementing appropriate interventions.
Conflict of Interest
None
Acknowledgment
The authors would like to acknowledge KIMS Hospital & Research Centre and the faculty of Surgery department along with the faculty of VIPS college for support throughout the study.
Supporting File
References
1) The integrated approach to the management of pain. Natl Inst Health Consens Dev Conf Consens Statement 1986;6(3):1-8.
2) Satoskar RS, Bhandarkar SD. Pharmacology and pharmacotherapeutics. Mumbai, India: Popular Prakashan; 2020.
3) Roshini A, Abhishek S, Ashwini K, et al. Prescribing patterns of analgesics in the postoperative peri-od of surgical interventions. Indo American Journal of Pharmaceutical Research 2015;5(7):2555-9.
4) Mohammed TH, Beegum IM, Perumal P. Prescribing pattern of analgesics in a tertiary care hos-pital. International Journal of PharmTech Research 2011;3(3):1521-1529.
5) Walker R, Whittlesea C. Clinical pharmacy and therapeutics. 5th ed. Churchill Livingstone; 2011.
6) Vallano A, Aguilera C, Arnau JM, et al. Management of postoperative pain in abdominal surgery in Spain. A multicentre drug utilization study. Br J Clin Pharmacol 1999;47(6):667-73.
7) Joshi S, Shetty Y, Panchal R, et al. An observation-al study to evaluate the prescription pattern of analgesics used in the perioperative period in a tert-iary care hospital. Perspect Clin Res 2021;12(3): 165-170.
8) Pogatzki-Zahn E, Kutschar P, Nestler N, et al. A prospective multicentre study to improve postoperative pain: identification of potentialities and problems. PLoS One 2015;10(11):e0143508.
9) Ramsay MA. Acute postoperative pain management. Proc (Bayl Univ Med Cent) 2000;13(3): 244-247.
10) Santos MD, Oh KS, Varrassi G, et al. Multimodal analgesia for postoperative pain in Asia: A review of evidence with clinical focus on dexketoprofen and tramadol/dexketoprofen fixed-dose combination. Signa Vitae 2021;17(6):1-7.
11) Marghoubi F, Nair MM, Kodandaram N. Analgesic Utilization Pattern in the Department of Surgery, Dr. BR Ambedkar Medical College and Hospital, Bangalore, India. PJMHS 2019;13(2):549.
12) Parulekar VV, Badar VA. Observing drug utilization trends of analgesics in indoor surgical patients in tertiary care teaching hospital. Asian J Pharm Clin Res 2020;13(5):47-50.
13) Chandrakantha T, Rajesh B, Neha K. Drug utilization pattern of analgesics among post-operative patients in a tertiary care hospital: A prospective study. Indian Journal of Pharmacy and Pharmacology 2020;6(4):137-41.
14) Barawade S, Gursale S. A study of drug utilization pattern of analgesics in postoperative patients of tertiary care hospital. MedPulse International Journal of Pharmacology 2017;1(2):28-32.