Vol No: 5 Issue No: 3 eISSN:
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Mrs. Ashika D, Associate Professor, A J Institute of Hospital Management, Mangalore, India.
2A J Institute of Hospital Management, Mangalore, Karnataka, India
3A J Institute of Hospital Management, Mangalore, Karnataka, India
4A J Institute of Hospital Management, Mangalore, Karnataka, India
*Corresponding Author:
Mrs. Ashika D, Associate Professor, A J Institute of Hospital Management, Mangalore, India., Email: ashiashika2705@gmail.com
Abstract
Background: Efficient operating theatre (OT) scheduling is essential for optimal resource utilization and patient outcomes. Delays in transferring patients from wards to the pre-op area significantly disrupt surgical schedules.
Aim: To identify and address factors causing delays in patient transfers to the pre-op area, distinguishing OT-related and ward-related issues.
Methods: This observational study conducted over a period of 14 days included 30 elective surgical cases. Data on transfer timing, delay reasons, and scheduling processes were collected and analyzed.
Results: Of the 30 cases, 20 experienced delays-11 due to OT-related factors (e.g., extended surgeries) and 9 due to ward-related factors (e.g., late bookings). Ten cases were shifted earlier than scheduled. Improvements in coordination, scheduling accuracy, and communication were identified as key interventions to reduce delays.
Conclusion: Prolonged surgeries and administrative inefficiencies were major contributors to delays. Addressing these factors through better coordination and monitoring can enhance OT utilization and patient care.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Efficient management of operating theatres (OTs) plays a critical role in ensuring optimal healthcare delivery. Operating theatres are among the most resource intensive units in a hospital, involving significant investments in infrastructure, skilled personnel, and equipment. As a result, inefficiencies in OT management can lead to financial losses, wasted resources, and compromised patient care.
Delays in transferring patients from the ward to the pre-operative (pre-op) area and subsequently to the OT are one of the most common challenges faced in hospital operations. These delays can disrupt carefully planned surgical schedules, resulting in cascading effects such as increased patient waiting times, reduced OT utilization, prolonged hospital stays, and increased healthcare costs.1,2 Furthermore, they may lead to patient dissatisfaction due to anxiety caused by unexpected waiting periods.
The process of preparing patients for surgery is complex and involves multiple stages of coordination. It begins with scheduling surgeries, ensuring completion of presurgery investigations, and confirming the availability of necessary resources such as surgeons, anaesthetists, and OT staff.3 Any breakdown or inefficiency in these stages can contribute to delays. For example, late bookings, miscommunication between departments, or inadequate pre-operative preparation are common causes of ward-related delays. On the other hand, prolonged previous surgeries or overlapping commitments of surgeons, such as outpatient department (OPD) consultations, can contribute to OT-related delays.4
In the face of increasing surgical demands and limited resources, addressing these delays has become more crucial than ever. Improving OT scheduling and patient transfer processes is not only essential for operational efficiency but also for enhancing the overall patient experience and clinical outcomes. By identifying the root causes of delays and implementing targeted interventions, hospitals can optimize their operations, reduce costs, and improve the quality of care delivered.
This study aimed to provide insights into the factors contributing to patient transfer delays in a tertiary care hospital, with a focus on distinguishing OT- and ward-related issues. By analyzing these factors and proposing actionable solutions, the study sought to improve OT scheduling efficiency and support better resource utilization in healthcare settings.
The primary aim was to analyse the process of transferring patients from the ward to the pre-op area and identify pre-surgery delays. Specific objectives included:
• Assessing the timing of patient transfers relative to scheduled surgery times.
• Identifying reasons for delays in patient transfers.
• Distinguishing between OT-related and ward-related causes of delays.
• Proposing strategies to minimize delays and improve OT scheduling efficiency.
Materials and Methods
This observational study was conducted to analyze the process of transferring patients from the ward to the pre-operative (pre-op) area and to identify factors contributing to delays. The study was carried out in the Operating Theatre (OT) Department of a tertiary care hospital for 14 consecutive days, between 7.45 am and 2 pm.
A total of 30 elective surgical cases were included in the study, selected using a convenience sampling method. The sample size was based on the average number of elective surgeries performed daily and the feasibility of conducting detailed, real-time observations during the study period. This number was considered adequate, as data saturation was achieved-recurrent patterns and delay factors were consistently observed across cases. Elective surgical cases scheduled during the study period were included, while emergency surgeries and cases cancelled before patient transfer were excluded.
Primary data were gathered through direct observations, and hospital records were used as secondary sources to cross-check and validate the recorded timings. The following steps were employed to ensure comprehensive data collection:
1. Identification of Cases: Elective surgeries scheduled during the study period were identified and included in the analysis.
2. Expected Transfer Time: The expected time for patient transfer to the pre-op area was defined as one hour before the scheduled surgery.
3. Shift Booking Time: The shift booking time was set at 15 minutes prior to the actual transfer of the patient.
4. Recording Timings:
• Time of booking the shift.
• Actual time of patient transfer from the ward to the pre-op area.
• Time elapsed between the expected transfer and actual transfer.
5. Documentation of Delays: Any delays were recorded and categorized into the following:
• OT-related delays: Factors such as prolonged surgeries or OT scheduling conflicts.
• Ward-related delays: Factors such as late booking of shifts or inadequate pre-surgery preparation.
The collected data were analyzed to:
1. Quantify Delays:
• Total number of cases with delays.
• Duration of delays categorized as:
Less than 30 minutes
Between 30 and 60 minutes
Greater than 60 minutes
2. Categorize Reasons for Delays:
• Ward-related delays: Administrative inefficiencies, same-day admissions requiring investigations, etc.
• OT-related delays: Prolonged surgeries, scheduling issues, etc.
3. Evaluate Early Transfers: Cases where patients were transferred earlier than expected.
Results
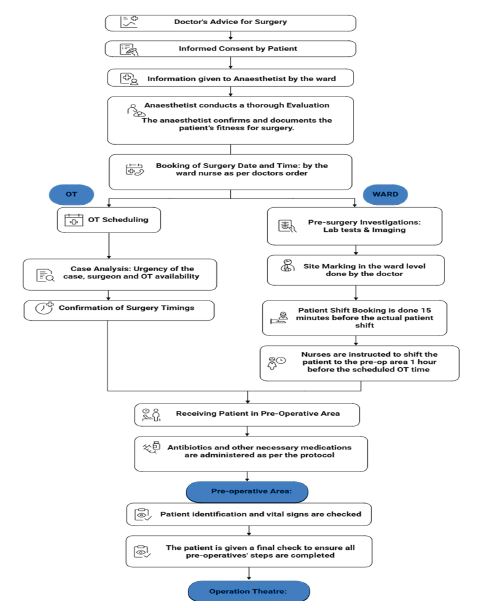
To analyze the factors contributing to delays in patient transfers to the pre-operative (pre-op) area, it was essential to first observe the existing operating theatre (OT) scheduling and transfer process. The workflow, as documented through direct observation, is illustrated in Figure 1 and served as the foundation for identifying delay patterns and their underlying causes.
Out of the 30 elective surgical cases analyzed, delays in patient transfers were observed in 20 cases, while 10 patients were shifted to the pre-op area earlier than the expected time. The expected time for patient transfer was defined as one hour before the scheduled surgery, with shift booking to be completed at least 15 minutes before the actual movement of the patient. Table 1 summarizes the distribution of delay durations and categorizes the underlying causes as OT-related or ward-related.
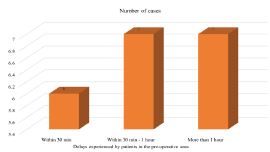
The delays were categorized into three intervals: less than 30 minutes (6 cases), 30 to 60 minutes (7 cases), and more than one hour (7 cases). Of these, 11 delays were attributed to OT-related causes, such as prolonged surgeries and surgeon unavailability, while nine were ward-related, mainly due to late bookings and same-day admissions requiring pending investigations. In the cases delayed by less than 30 minutes, one was OT-related and five were ward-related (including four due to delayed bookings and one due to a pending investigation). Among the seven cases delayed by 30-60 minutes, five were OT-related and two were ward-related. In the seven cases delayed by over an hour, five were due to OT-related reasons and two were linked to ward-side delays.
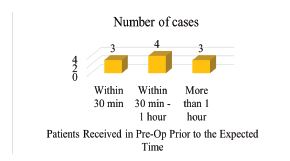
Table 2 presents a summary of the 10 cases where patients were transferred earlier than expected, along with contributing factors.
Regarding the time taken to shift patients from the pre-op area into the OT, 23 of the 30 cases were transferred within one hour of their arrival, suggesting a generally streamlined transition process. However, in seven cases, the transfer took more than an hour. Of these, six delays were due to the extended durations of earlier surgeries, which disrupted the schedule. One case involved a miscommunication, where the patient was sent to the OT without proper information, pointing to a gap in interdepartmental coordination.
The data provided in Figure 2 showcases the delays experienced by patients in the pre-operative (pre- op) area, exceeding the expected arrival time. The expected time for patients to arrive in the pre-op area was set at one hour before their scheduled surgery, with a shift booking time of 15 minutes before patient shifting.
Figure 3 highlights the 10 cases where patients were transferred to the pre-op area earlier than expected. Three patients arrived less than 30 minutes early two due to early booking by ward staff and one because the previous OT case finished ahead of time. Four patients arrived 30 minutes to one hour early three due to early completion of prior surgeries and one due to a shift initiated by a referring doctor without system confirmation.The remaining three cases arrived more than one hour early, with similar contributing factors.
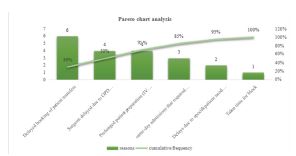
Figure 4, a Pareto analysis, reveals that approximately 70% of delays stemmed from just three primary causes: delayed booking of patient transfers, surgeon delays due to OPD commitments, and prolonged preoperative preparation. This highlights the importance of addressing a few high-impact areas to significantly reduce overall delays.
The findings indicate that improving OT efficiency requires targeted interventions. These include streamlining the booking process by training all concerned staff, ensuring proper communication, and avoiding last minute errors. Adjusting surgeon schedules to reduce conflicts with OPD duties or assigning dedicated teams to manage either responsibility could further minimize delays. Enhancing preoperative readiness through timely investigations, standardized checklists, and better coordination is also critical. Additionally, implementing continuous monitoring, regular audits, and feedback mechanisms can help identify trends and enforce compliance with best practices. Periodic staff training will further reinforce these protocols and promote a culture of operational discipline.
Discussion
Efficient operation theatre (OT) utilization is essential for optimal hospital functioning, patient safety, and resource management. Delays in scheduled surgeries disrupt surgical workflows, prolong patient waiting times, and contribute to adverse clinical outcomes. In the present study, several factors contributing to OT delays were identified, consistent with the findings from earlier research conducted in different healthcare settings.
A prospective study in a 1000-bedded rural tertiary care hospital reported that incomplete preoperative preparation, late arrival of patients, and unavailability of essential surgical equipment were the predominant causes of OT delays.1 This aligns with the present study, where similar operational issues contributed to the postponement of scheduled surgeries.
A study conducted at a Nigerian teaching hospital reported that delayed arrival of surgeons and patients was a major contributor to late surgical start times.3 These findings resonate with the present study, underscoring the universal challenges faced by healthcare facilities in managing OT schedules efficiently.
The current study highlighted patient transportation delays as a significant contributor to OT inefficiency. Halder et al., observed that delays in transferring patients from the wards to the operation theatre complex adversely affected OT start times and resulted in cumulative scheduling disruptions.5
An observational study from Bangladesh further explored reasons for delays in turnover time in the OT and found that inadequate coordination among the surgical, anaesthesia, and housekeeping teams contributed significantly.6 Similar patterns were observed in the current study, where inefficient communication resulted in extended turnover times.
Additional studies have corroborated that optimizing OT scheduling and improving interdepartmental cordination can significantly enhance OT efficiency.7,8 Furthermore, the study highlighted that adherence to scheduled start times and effective preoperative planning are critical factors for influencing OT productivity.9
Implementing remedial measures such as dedicated patient transport teams, real-time OT scheduling software, and periodic audits of delays could help in minimizing avoidable delays and improving overall surgical throughput. As demonstrated in similar interventions by previous studies, operational modifications and process standardization can lead to substantial improvements in OT efficiency and patient satisfaction.10,11
Conclusion
Addressing the identified delays requires a multi-faceted approach that combines better scheduling, enhanced communication, continuous monitoring, and ongoing staff training. By focusing on the primary causes of delays such as booking inefficiencies, surgeon availability, and preoperative preparation the hospital can significantly reduce the frequency and impact of these delays.
The implementation of streamlined processes, effective time management, and continuous improvement mechanisms will ensure that patients are transferred to the pre-op area and the OT on time. This will not only enhance the overall efficiency of OT utilization but also improve patient care and outcomes. The study highlights the importance of collaboration among different departments within the hospital and the need for a coordinated approach to managing OT schedules and patient transfers.
By addressing these areas and implementing the recommended strategies, the hospital can achieve more timely surgical procedures, reduce patient wait times, and ensure better utilization of the operating theatres. Continuous evaluation and adaptation of these processes will be crucial in maintaining efficiency and improving patient care in the long term.
Conflict of interest
Nil
Acknowledgement
NA
Supporting File
References
1. Naik SV, Dhulkhed VK, Shinde RH. A prospective study on operation theater utilization time and most common causes of delays and cancellations of scheduled surgeries in a 1000-bedded tertiary care rural hospital with a view to optimize the utilization of operation theater. Anesth Essays Res 2018;12(4):797-802.
2. Denton B, Viapiano J, Vogl A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag Sci 2007;10:13-24.
3. Okeke CJ, Okorie CO, Ojewola RW, et al. Delay of surgery start time: experience in a Nigerian teaching hospital. Niger J Surg 2020;26(2):110-6.
4. Dexter F, Shi P, Epstein RH. Descriptive study of case scheduling and cancellations within 1 week of the day of surgery. Anesth Analg 2012;115(5): 1188-95.
5. Haldar R, Gupta D, Pandey H, et al. Patient transportation delays and effects on operation theatre's efficiency: A study for problem analysis and remedial measures. Anesth Essays Res 2019;13(3):554-9.
6. Kumar M, Malhotra S. Reasons for delay in turn-over time in operating room an observational study. Bangladesh J Med Sci 2017;16(2):245-51.
7. Talati S, Gupta AK, Kumar A, et al. An analysis of time utilization and cancellations of scheduled cas-es in the main operation theater complex of a tertiary care teaching institute of North India. J Postgrad Med 2015;61(1):3-8.
8. Vinukondaiah K, Ananthakrishnan N, Ravishankar M. Audit of operation theatre utilization in a general hospital. Natl Med J India 2000;13(3):118-21.
9. Bhattacharyya T, Vrahas MS, Morrison SM, et al. The value of the dedicated orthopaedic trauma op-erating room. J Trauma 2006;60(6):1336-41.
10. Park HS, Kim SH, Bong MR, et al. Optimization of the operating room scheduling process for im-proving efficiency in a tertiary hospital. J Med Syst 2020;44:1-7.
11. Dexter F, Macario A, Traub RD, et al. An operat-ing room scheduling strategy to maximize the use of operating room block time: computer simulation of patient scheduling and survey of patients' preferences for surgical waiting time. Anesth Analg 1999;89(1):7-20.