RGUHS Nat. J. Pub. Heal. Sci Vol No: 10 Issue No: 4 eISSN: 2584-0460
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Sushma Shekar Chandrashekar, Postgraduate, Department of Community Medicine, Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
2Department of Community Medicine, Bangalore Medical College and Research Institute (BMCRI), Bengaluru, Karnataka, India
3Department of Community Medicine, Bangalore Medical College and Research Institute (BMCRI), Bengaluru, Karnataka, India
4Department of Community Medicine, Bangalore Medical College and Research Institute (BMCRI), Bengaluru, Karnataka, India
5Department of Community Medicine, Bangalore Medical College and Research Institute (BMCRI), Bengaluru, Karnataka, India
*Corresponding Author:
Dr. Sushma Shekar Chandrashekar, Postgraduate, Department of Community Medicine, Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India., Email: csushmashekar@gmail.com
Abstract
Background: Diabetes is a major global health concern, with India carrying a large share of the burden. Many remain unaware of their condition, leading to serious complications. While research often focuses on prevalence and risk factors, quality of life, particularly in low-resource urban areas, is less studied.
Aim: To assess the quality of life and its associated factors in type 2 diabetes patients in an urban slum in Bengaluru.
Methods: A community-based cross-sectional study was conducted in an urban slum in Bengaluru in 2024. A total of 173 patients with type 2 diabetes were selected through cluster sampling and interviewed using a semi-structured questionnaire and the WHOQOL-BREF scale after obtaining written informed consent.
Results: The participants had an average age of 56.5 ± 8.96 years, with half being illiterate. A majority were unemployed (51.4%), lived in nuclear families (66.5%), and belonged to the middle socioeconomic class (46.8%). Mean Quality of Life (QoL) scores were 49.94 ± 17.88 (physical), 51.72 ± 15.18 (psychological), 53.23 ± 19.23 (social), and 55.64 ± 14.3 (environmental). Reduced QoL was associated with increasing age, hypertension, longer diabetes duration, and lower socioeconomic status.
Conclusions: The study found that quality of life in individuals with type 2 diabetes living in an urban slum was influenced by age, economic status, comorbid conditions like hypertension, and how long they had the disease. Those who were older had additional health issues or belonged to lower-income groups and reported lower QoL, underscoring the importance of tailored healthcare and social support in these contexts.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Diabetes mellitus (DM) is a chronic metabolic condition characterized by persistent hyperglycemia, which over time can lead to complications affecting vital organs such as the heart, kidneys, eyes, nerves, and blood vessels.1 Type 2 diabetes is the most prevalent form, particularly among adults, and arises due to insulin resistance or inadequate insulin production.2 Alongside its medical impact, diabetes significantly affects individuals’ daily functioning and psychological well-being, making quality of life (QoL) a crucial aspect in managing the disease.3
Worldwide, over 422 million people live with diabetes, predominantly in low and middle-income countries.4 India, often recognized as the “diabetes capital,” contributes approximately 17% of the global diabetic population.5 An estimated 77 million adults in India have type 2 diabetes, with nearly 25 million more classified as pre-diabetic. A large proportion remains undiagnosed, which increases the likelihood of complications and adversely affects their quality of life.6
With the high prevalence of diabetes in India, significant research happens to improve the quality of care for the patients, however most of the studies related to diabetes mellitus were done concerning prevalence of the disease and its association with the risk factors, self-care and medication adherence, only few studies are on the psychological effects and QoL of diabetic patients.7 QoL is how good or bad a person feels their life to be. Thus, the purpose of this study was to assess QoL among patients with type 2 diabetes mellitus in an urban slum area of Bengaluru.
Materials and Methods
In 2024, a community-based cross-sectional study was conducted among individuals with type 2 diabetes residing in an urban slum of Bengaluru. A total of 173 participants were selected via cluster sampling. The sample size was determined based on the study by Pattankar et al.8 Adults aged 18 years and above with a diabetes duration of more than six months were included, while those who were terminally ill or mentally impaired were excluded. Participants were selected using a random number generator, and data were collected using a semi-structured, pre-tested questionnaire and the WHOQOL-BREF scale.
Assessment Tools:
a. Semi-structured and pretested questionnaire- socio-demographic details, psycho-cultural factors.
b. WHOQOL – BREF scale: This questionnaire consists of 26 items and 4 QoL domains: Domain 1- Physical health (7 questions), Domain 2- Psychological health (6 items), Domain 3- Social relationships (3 items), and Domain 4- Environment (8 items).9
Statistical Analysis: The data was entered into Microsoft Excel and analyzed using SPSS version 21.0. Socio-demographic information and other relevant characteristics were summarized using descriptive statistics, including frequencies, percentages, and mean values. Linear regression analysis was used to investigate associations between variables. The findings were presented as tables, charts, and graphs.
Results
A total of 173 patients with type 2 diabetes mellitus participated in the study. The mean age of the participants was 56.55 ± 8.96 years, with ages ranging from 39 to 80 years. The majority of participants were female (73.4%), while 26.6% were male. Married participants accounted for 54.9%, followed by widowed individuals at 40.5% and divorced individuals at 4.6%. In terms of religion, 75.7% were Hindu, 19.7% were Muslim, and the remainder were Christian. The majority of them were illiterate (54.3%), and only 4.6% had studied up to the pre-university level (PUC). A total of 51.4% of participants were unemployed. Regarding family type, 66.5% were nuclear families, 23.7% were three-generation families, and 9.8% were joint families. Based on the Modified B.G. Prasad Classification (2024), 46.8% participants belonged to the middle class, and 24.9% to the lower socio-economic class (Table 1).
About 53.8% of participants were diagnosed with diabetes following complications. In terms of disease duration, 54.9% had diabetes for 1–5 years, while only 3.5% had lived with the condition for 16–20 years. Regular use of anti-diabetic medication was reported by 78.6% of participants. Hypertension was present in 53.8%, chronic kidney disease in 2.3%, cardiovascular disease in 8.1%, and diabetic retinopathy in 2.3%. Based on BMI, 64.2% were obese and 1.7% were underweight. Tobacco use was reported by 14.5% and alcohol consumption by 6.9%.
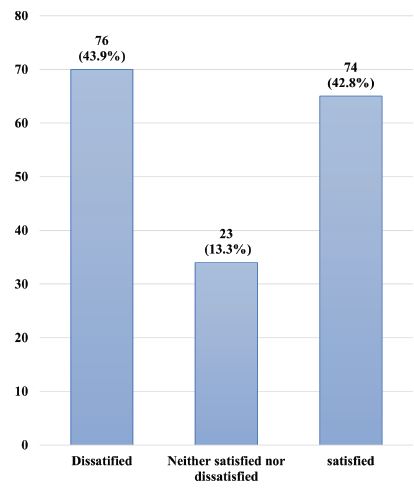
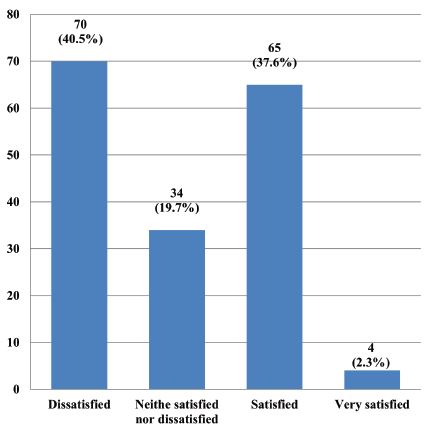
Of the participants, 43.9% reported poor perceived quality of life, 13.3% reported neither poor nor good, and 42.8% reported good perceived quality of life (Figure 1). Only 2.3% were very satisfied with their health, while 40.5% were dissatisfied (Figure 2). The mean transformed scores across the WHOQOL-BREF domains were as follows: physical domain – 49.94 ± 17.88; psychological domain – 51.72 ± 15.18; social domain – 53.23 ± 19.23; and environmental domain – 55.65 ± 14.30. In terms of domain-specific QoL, 43.9% had poor QoL in the physical domain, 37.6% in the psychological domain, 29.5% in the social domain, and 21.4% in the environmental domain (Table 2). Older age, lower education levels, hypertension, longer duration of diabetes (6–10 years), belonging to a nuclear family, and lower socio-economic status were significantly associated with poorer perceived QoL. In contrast, being unmarried, unemployed, or self-employed, and having stronger social relationships were associated with a better perceived quality of life (Table 3).
Discussion
The socio-demographic profile of the participants reveals a predominance of females (73.4%), consistent with findings from studies by John et al., and Majumdar et al., in which women formed the majority of the diabetic sample, particularly in community-based settings.10,11 The mean age of the participants was 56.5 years, closely resembling the findings of Patel et al., and Pattankar et al., reflecting the common mid-to-late adult onset of type 2 diabetes.12,8
A majority of the participants were illiterate (54.3%) and unemployed (51.4%), highlighting the socioeconomically disadvantaged profile of the urban slum population. A similar educational distribution was reported in the study by Gara et al., reinforcing the link between limited education and vulnerability to chronic diseases and their complications.13 Most belonged to nuclear families, a trend observed in urban India amid ongoing shifts in family structure. Regarding socioeconomic status, 46.8% were from the middle class, which contrasts with rural studies such as Somappa et al., which report higher proportions from lower classes, possibly due to urban proximity to resources.14
In terms of QoL scores, the current study observed the lowest mean transformed score in the physical health domain (49.94 ± 17.88), followed by the psychological domain (51.72 ± 15.18), social relationships (53.23 ± 19.23), and the highest in the environmental domain (55.64 ± 14.30). These scores suggest that physical limitations and mental health concerns are the most affected areas for diabetics in slum populations. These findings are consistent with those of Manjunath et al., and Jing et al., both of which reported reduced physical and psychological QoL among diabetics, particularly in resource-poor settings.15,16
A relatively better score in the environmental domain could reflect supportive community infrastructure or the availability of government services in the urban slum area. However, the mean scores across all domains remain below optimal thresholds, similar to those reported by Patel et al. and Aarthy et al., who found that the overall QoL of diabetic patients in India tends to be lower than global averages, particularly among lower-income groups.12,16
Regression analysis revealed several important predictors of QoL. Age was significantly negatively associated with QoL, indicating declining QoL with increasing age, similar to patterns observed in the meta-analysis by Jing et al.17 Among the WHOQOL-BREF domains, social relationships had a statistically significant positive association with perceived QoL, emphasizing the critical role of interpersonal support systems. Environmental QoL was marginally significant (P = 0.0500), suggesting that community or infrastructural aspects modestly impact overall well-being.
Education emerged as a strong determinant of QoL, with illiterate individuals reporting significantly lower QoL than those educated up to PUC. This finding aligns with studies by Bahety et al., and Gara et al., highlighting how education influences disease awareness, self-care practices, and health-seeking behavior.18,13 Participants from nuclear families also had significantly lower QoL scores, which supports findings by Majumdar et al. that joint family structures offer protective psychosocial benefits in chronic illness.11
Socioeconomic status showed a strong inverse relationship with QoL. Participants from lower-middle and middle classes had significantly lower QoL compared to those from upper-middle class backgrounds, consistent with findings from Aarthy et al.,and Pattankar et al.16,8 Comorbid hypertension and longer diabetes duration (6–10 years: B = -0.703, P< 0.0001) also significantly reduced QoL, affirming the burden of chronic complications noted in the DAWN study by Peyrot et al.7 In this study, non-adherent participants reported significantly higher QoL (B = 0.935, P< 0.0001), possibly due to milder disease or lower perceived burden, leading to less need for strict adherence. Similar findings were reported by Bahety et al., while other studies, such as Peyrot et al. and Jain et al., linked poor adherence to lower QoL.18,7,19 This contrast may reflect differences in disease severity, awareness, and self-reporting, suggesting that QoL is influenced more by perceived health status than adherence alone.
Conclusion
This study shows that quality of life in type 2 diabetes patients from a Bengaluru urban slum is affected by factors like lower education, older age, nuclear families, hypertension, longer disease duration, and low socio-economic status. Social relationships improved overall QoL, while non-adherence to medication was linked to higher QoL, possibly due to lower perceived illness. The findings emphasize the need for comprehensive care addressing social support, education, and comorbidities, tailored to the unique challenges of slum populations.
Conflicts of Interest
There are no conflicts of interest
Acknowledgement
We sincerely thank the Institute for its support and facilitation throughout the research process. Our heartfelt appreciation also goes to the community health workers and Accredited Social Health Activists (ASHA) for their invaluable assistance in data collection.
Supporting File
References
1. World Health Organization. Diabetes [Internet] 2024 [cited 2025 Mar 7]. Available from: https://www. who.int/news-room/fact-sheets/detail/diabetes.
2. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014 Jan;37 Suppl 1:S81-90.
3. Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes/metabolism research and reviews. 1999;15(3):205-18.
4. International Diabetes Federation. Diabetes around the World in 2025 [Internet]. IDF Diabetes Atlas. International Diabetes Federation. 2025. [cited 2025 Mar 7] Available from: https://diabetesatlas. org/.
5. Anjana RM, Deepa M, Pradeepa R, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR–INDIAB population-based cross-sectional study. The lancet Diabetes & endocrinology 2017;5(8):585-96.
6. World Health Organization. Depression [Internet]. WHO India [cited 2025 Mar 7]. Available from: https://www.who.int/india/health-topics/depression.
7. Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross‐National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabetic Medicine 2005;22(10):1379-85.
8. Pattankar TP, Patil SS. Assessment of Quality of Life among Known Type 2 Diabetics–A Community Based Cross Sectional Study in North Karnataka. National Journal of Community Medicine 2019;10(07):429-34.
9. Abbasi-Ghahramanloo A, Soltani-Kermanshahi M, Mansori K, et al. Comparison of SF-36 and WHOQoL-BREF in measuring quality of life in patients with type 2 diabetes. International Journal of General Medicine 2020:497-506.
10. John R, Pise S, Chaudhari L, Deshpande PR. Evaluation of quality of life in type 2 diabetes mellitus patients using quality of life instrument for indian diabetic patients: A cross-sectional study. Journal of Midlife Health 2019;10(2):81-8.
11. Majumdar A, Pavithra G. Quality of life (QOL) and its associated factors using WHOQOL-BREF among elderly in urban Puducherry, India. Journal of Clinical and Diagnostic Research: JCDR 2014;8(1):54.
12. Patel B, Oza B, Patel K, Malhotra S, Patel V. Health related quality of life in type-2 diabetic patients in Western India using World Health Organization Quality of Life–BREF and appraisal of diabetes scale. International Journal of Diabetes in Developing Countries 2014;34:100-7.
13. Gara HK, Panda K, Vanamali DR. WHOQOL-BREF as a tool for evaluation of quality of life and its predictors in type-2 diabetics: a cross-sectional study in Visakhapatnam, Andhra Pradesh. Assam J Intern Med 2020;10(1):15.
14. Somappa HK, Venkatesha M, Prasad R. Quality of life assessment among type 2 diabetic patients in rural tertiary centre. Int J Med Sci Public Health 2014;3(4):415-7.
15. Manjunath K, Christopher P, Gopichandran V, Rakesh PS, George K, Prasad JH. Quality of life of a patient with type 2 diabetes: a cross-sectional study in rural South India. Journal of Family Medicine and Primary Care 2014;3(4):396-9.
16. Aarthy R, Mikocka-Walus A, Pradeepa R, Anjana RM, Mohan V, Aston-Mourney K. Quality of life and diabetes in India: a scoping review. Indian Journal of Endocrinology and Metabolism. 2021;25(5):365- 80.
17. Jing X, Chen J, Dong Y, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health and quality of life outcomes 2018;16:1-4.
18. Bahety P, Agarwal G, Khandelwal D, et al. Occurrence and predictors of depression and poor quality of life among patients with type-2 diabetes: a Northern India perspective. Indian Journal of Endocrinology and Metabolism 2017;21(4):564-9.
19. Jain A, Sharmab R, Yadavc N, Chaudhary P, Jainc G, Maanju M. Quality of life and its association with insomnia and clinical variables in type 2 diabetes. Journal of Egyptian Public Health Association 2017;92(1):52-9.