RGUHS Nat. J. Pub. Heal. Sci Vol No: 10 Issue No: 4 eISSN: 2584-0460
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Department of Community Medicine, Jawahar Lal Nehru Medical College, AMU, Aligarh, UP, India
2Department of Community Medicine, VALASMC, Etah, UP, India
3Department of Community Medicine, Jawahar Lal Nehru Medical College, AMU, Aligarh, UP, India
4Department of Community Medicine, Jawahar Lal Nehru Medical College, AMU, Aligarh, UP, India
5Department of Community Medicine, Jawahar Lal Nehru Medical College, AMU, Aligarh, UP, India
6Dr. Fareha Husain, Assistant Professor, Department of Physiology, VALASMC, Etah, UP, India.
*Corresponding Author:
Dr. Fareha Husain, Assistant Professor, Department of Physiology, VALASMC, Etah, UP, India., Email: drfarehahusain1@gmail.com
Abstract
Background: Depression is a common comorbidity in patients with diabetes mellitus that often remains underdiagnosed and untreated. With the rising burden of diabetes in India, understanding the prevalence and determinants of depression among diabetic patients is crucial for developing integrated care approaches.
Objective: To estimate the proportion of adults in the urban slums of Bengaluru who have availed preventive health checkups and to identify the motivators and barriers influencing their utilization.
Methods: This cross-sectional study included 241 patients with type 2 diabetes mellitus from four field practice areas of JNMCH, Aligarh. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9). Clinicodemographic characteristics were collected using a predesigned semi-structured questionnaire. Chi-square test and binary logistic regression were employed to analyze associations between variables.
Results: The mean age of participants was 53.95 ± 12.10 years, with 62.7% being female. Moderate to moderately severe depression was present in 31.9% of patients (26.1% moderate, 5.8% moderately severe). Significant associations were found between depression and several factors: female gender (42.4% vs 17.8% in males, P<0.001), middle age group of 41-60 years (adjusted OR: 6.7, 95% CI: 2.6-21.1, P=0.001), and presence of diabetes complications (adjusted OR: 3.3, 95% CI: 1.6-6.8, P=0.001). Duration of diabetes >10 years showed significant association in unadjusted analysis (OR: 3.1, 95% CI: 1.5-6.4) but became non-significant after adjustment.
Conclusion: The high prevalence of depression among diabetic patients, particularly in specific demographic groups, emphasizes the need for routine depression screening in diabetes care settings. Special attention should be paid to middle-aged patients, women, and those with complications. Implementation of integrated care models incorporating mental health services into routine diabetes care could significantly improve patient outcomes.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
According to the International Diabetes Federation (IDF), an estimated 537 million adults aged 20-79 years (10.5% of the global population) are currently living with diabetes. By 2030, 643 million, and by 2045, 783 million people aged 20-79 years are projected to live with diabetes.1 With improvement in the quality of care and provision of effective treatments, the survival of patients with diabetes has increased and this is contributing to a rise in people living with comorbid conditions, also known as multiple long-term conditions (MLTC) or multimorbidities.2 One of the major contributors to MLTC among patients with diabetes is purported to be mental health conditions, with depression being particularly prominent.3 Depression remains underdiagnosed and untreated in a significant number of patients with diabetes.4 These comorbid conditions are also likely to lead to poor medication adherence and, consequently, inadequate glycaemic control.
In India, the World Health Organization (WHO) has estimated that 77 million people aged above 18 are living with type 2 diabetes mellitus, while nearly 25 million have prediabetes.5 Given this high burden, the prevalence of comorbid conditions-particularly depression-is also likely to be substantial. In this study, we aimed to estimate the prevalence of depression among individuals with diabetes and its clinicodemographic associates. We also emphasize the need for integrated care for patients with diabetes to improve outcomes.
Materials and Methods
This cross-sectional study was conducted in four field practice areas of Urban Health Training Centre (UHTC), JNMCH, Aligarh, namely Firdaus Nagar, Nagla Qila, Patwari Nagla, Shahanshabad. A meticulous search of all diabetes mellitus patients in the study area was carried out with the help of Medical Social Workers (MSWs). After due consideration of inclusion and exclusion criteria, 241 patients were included in the study. Predesigned semi-structured questionnaire was used to obtain data regarding clinicodemographic characteristics. Patient Health Questionnaire-9 (PHQ-9) was used to assess depression.6 Depression was classified on the basis of total scores as, no (0-4), mild (5-9), moderate (10-14), moderately-severe (15-19) and severe (19- 27). Diabetic patients aged 18 years and above were included in the study. Diabetes mellitus was diagnosed based on self-reported medical history, biochemical test results, and use of medication. Patients with type 1 diabetes mellitus, gestational diabetes, endocrine disorders, chronic corticosteroid use, severe illness precluding response, or those who did not provide consent were excluded from the study.
Data obtained were entered analyzed using Statistical Package for Social Science (SPSS) version 20.0. Chi-square test was used to study the association between clinicodemographic characteristics and depression. Binary logistic regression model was employed for quantifying the effect of predictors of depression amongst type 2 diabetes mellitus patients. Clearance for the study was obtained from Institutional Ethics Committee, JNMCH.
Results
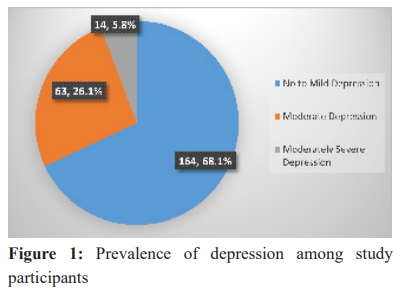
A total of 241 patients were included in the study. The mean age was 53.95 ± 12.10 years, with 151 (62.7%) females and 90 (37.3%) males. The prevalence of moderately severe depression was 5.8% (n=14), while moderate depression was observed in 26.1% (n=63). The majority of patients fell into the no-to-mild depression category (n=164; 68.1%). Notably, no patient in our study had severe depression (Figure 1).
Clinicodemographic Associates of Depression
The clinicodemographic associates of depression are presented in Table 1. The prevalence of moderate to moderately severe depression was significantly higher in females compared to males (42.4% vs 17.8%; P <.001). The proportion of patients with significant depression was highest in the 41-60 year age group (41.9%), compared with those aged >60 years (25.7%) and ≤ 40 years (11.9%). This difference was statistically significant (P =.001). Religion, level of education, marital status, and socioeconomic status were not found to be associated with depression.
Amongst the clinical factors, longer duration of diabetes was significantly associated with depression (P=.003; Table 1). The proportion of patients with depression was significantly higher among those who were overweight (40%) or obese (36.9%) compared with those of normal weight (19.6%) (P =.046). Patients with one or more diabetes-related complications were also more likely to have depression than those without complications (44.85 vs 22.4%: P <.001). Patients with a history of tobacco consumption were less likely to have depression compared with non-users (16.7% vs 38.7%; P =.002).
Univariate and Multivariate Regression Analysis
Univariate and multivariate binary logistic regression was carried out for variables with a P value <0.2 in the association table and the result is presented in Table 2. On univariate analysis, female gender, age group, duration of diabetes, BMI, absence of tobacco use, and diabetes-related complications were found to be significant predictors of depression (Table 2).
On multivariate analysis, however, only age 41-60 years (OR 6.7, 95% CI: 2.6-21.1; P =.001), use of tobacco (OR 0.2, 95% CI: 0.1-0.4; P <.001) and diabetes-related complications (OR 3.3, 95% CI: 1.6-6.8; P =.001) remained significant predictors of depression. Gender, which was a statistically significant predictor on univariate analysis, was not significant on multivariate analysis (Table 2). This may be explained by the confounding effect of age, as the majority of females in our study belonged to higher age group compared to males. Similarly, duration of diabetes, although significant on univariate analysis, was not significant on multivariate analysis (Table 2). This may again be attributed to the confounding effect of age, since older patients also tended to have a longer duration of diabetes.
Discussion
This cross-sectional study conducted in the field practice areas of Department of Community Medicine, JNMCH, Aligarh, provides important insights into the prevalence and determinants of depression among patients with type 2 diabetes mellitus. Our findings revealed that nearly one-third (31.9%) of diabetic patients experienced moderate to moderately severe depression, with 26.1% showing moderate depression and 5.8% exhibiting moderately severe depression. This significant prevalence underscores the considerable mental health burden among diabetic patients and aligns with various national and international studies that have reported depression prevalence ranging from 20% to 40% among diabetic populations. The DAWN study which was a large cross-sectional study from 13 different countries including Asia, Europe, Australia, and North America concluded that 41% of the adults with type 2 diabetes mellitus had poor psychosocial well-being. Asia was represented by India and Japan in this study.7 A study conducted in Malaysia, in a group of 169 type 2 diabetes mellitus patients, reported a prevalence of anxiety in 31.4% and depression in 40.3% of patients.8 Another study from India in people with diabetes within urban populations estimated depression prevalence to be approximately 41%.9 This high occurrence may be attributed to the apprehension of the future complications, psychological and social demands, and life-long lifestyle changes that are required for patients diagnosed with diabetes.
The gender distribution of depression in our study population revealed a striking disparity, with females showing significantly higher rates of moderate to moderately severe depression (42.4%) compared to males (17.8%). This finding is consistent with the general trend observed in depression epidemiology, where women typically show higher vulnerability to depression. A study among patients attending the OPD at a tertiary care hospital in Colombo, the capital city of Sri Lanka reported females being more affected than males (25.4% versus 18.7%).10 Many such studies conducted on similar populations revealed similar results.11,12 Two studies from India have also underscored this finding.13,14 The higher prevalence among women might be attributed to various factors including hormonal differences, societal pressures, domestic responsibilities, and potentially lower access to mental health resources in the Indian context.
Age emerged as a significant predictor of depression in our study population, with the middle-aged group (41-60 years) showing the highest risk (adjusted OR: 6.7, 95% CI: 2.6-21.1). This age group's vulnerability might be explained by the culmination of multiple stressors including peak family responsibilities, career demands, and the challenges of managing a chronic condition. The lower prevalence in the younger age group (≤40 years) might reflect better adaptive capabilities and support systems, while the relatively lower rates in the elderly (>60 years) could suggest the development of better coping mechanisms over time.
A particularly noteworthy finding was the strong association between diabetes complications and depression (adjusted OR: 3.3, 95% CI: 1.6-6.8). Some studies have reported association of depression with comorbid conditions among diabetics.15,16 This relationship likely operates bidirectionally - complications may lead to increased psychological distress, while depression might contribute to poor disease management and subsequent complications. This finding emphasizes the critical need for early screening and management of both conditions to prevent a detrimental cycle of worsening physical and mental health.
The duration of diabetes showed a significant association with depression in the unadjusted analysis, with patients having diabetes for more than 10 years showing higher odds of depression (OR: 3.1, 95% CI: 1.5-6.4). Although this association became non-significant after adjustment, it highlights the potential cumulative psychological burden of managing a chronic condition over an extended period. This finding suggests the need for sustained psychological support throughout the disease course, not just at diagnosis.
Our study revealed an interesting association between BMI and depression, with both overweight and obese individuals showing higher odds of depression compared to those with normal BMI in the unadjusted analysis. This relationship, while attenuated in the adjusted analysis, points to the complex interplay between metabolic health and mental well-being.15 Obesity might contribute to depression through multiple pathways including body image issues, reduced physical activity, and social stigma, while depression might lead to poor dietary choices and reduced physical activity, creating a vicious cycle.
An unexpected finding was the apparent protective effect of tobacco consumption against depression (adjusted OR: 0.2, 95% CI: 0.1-0.4). However, this finding should be interpreted with caution as it might reflect temporary mood modification effects of nicotine rather than true protection against depression.
Interestingly, our study found no significant association between depression and several conventional sociodemographic factors such as education, religion, and socioeconomic status. This suggests that the psychological impact of diabetes might transcend these social determinants, affecting individuals across different social strata similarly. However, since other studies have reported an association with lower education level,7,17 this finding might also reflect the relatively homogeneous nature of our study population and warrants further investigation in more diverse settings.
Conclusion
This study highlights the substantial burden of depression among patients with type 2 diabetes mellitus, with nearly one-third of the participants experiencing moderate to moderately severe depressive symptoms. The high prevalence underscores the need to integrate mental health evaluation into routine diabetes care. Notably, depression was more common among females, middle-aged individuals, and those with diabetes-related complications—indicating specific subgroups that may benefit from targeted psychological interventions.
The strong association between depression and complications of diabetes, as well as its relationship with disease duration and BMI, suggests that psychological distress may both result from and contribute to poorer disease outcomes. These findings reinforce the importance of a multidisciplinary approach that addresses both physical and psychological aspects of diabetes management.
The unexpected finding regarding tobacco use and depression, while intriguing, must be interpreted with caution and requires deeper investigation.
Thus, our study emphasizes that mental health, especially depression, is a significant but often overlooked comorbidity in patients with type 2 diabetes. Routine screening, early identification, and integrated management of depression should be prioritized to improve both psychological well-being and long-term diabetes outcomes.
Limitations
Several limitations of our study should be acknowledged. The cross-sectional design prevents establishment of causal (or temporal) relationships between diabetes and depression. The relatively small sample size and localized study setting might limit the generalizability of our findings to other populations. Additionally, the use of self-reported measures might have introduced recall bias.
Future studies should focus on longitudinal designs to better understand the temporal relationship between diabetes and depression, investigation of intervention strategies for this dual burden, and also exploration of protective interventions that might help in preventing depression among diabetic patients. Studies examining the cost-effectiveness of integrated care models would also be valuable in informing policy decisions, particularly in Indian context where both diabetes and depression are surging.
Conflict of Interest
None
Source of Funding
Nil
Ethical clearance
The study was approved by the Institutional Ethics Committee, Jawaharlal Nehru Medical College and Hospital (JNMCH), Aligarh Muslim University (AMU), Aligarh.
Supporting File
References
- International Diabetes Federation (IDF). IDF Diabetes Atlas. 2021; Available from: IDF Diabetes Atlas 2021 | IDF Diabetes Atlas [Accessed on 20th October, 2024].
- Multimorbidity: clinical assessment and management: NICE guideline [NG56], 2016. Available from https:// www.nice. org.uk/guidance/NG56 [Accessed on 20th October, 2023]
- Sunny AK, Khanal VK, Sah RB, Ghimire A. Depression among people living with type 2 diabetes in an urbanizing community of Nepal. PLoS one 2019;14:e0218119.
- Katon WJ. The Comorbidity of Diabetes Mellitus and Depression. Am J Med 2008;121(11):S8-15.
- WHO. Diabetes in India.2023; Available from: Diabetes - India [Accessed on: 25th October, 2024]
- Standford Medical Education. Patient Health Questionnaire. Available from: Patient Health Questionnaire (PHQ-9)
- Peyrot M, Rubin RR, Siminerio LM. Results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabetes Care 2006;29(6):1256-1262.
- Ganasegeran K, Renganathan P, Manaf RA, Al-Dubai SAR. Factors associated with anxiety and depression among type 2 diabetes outpatients in Malaysia: a descriptive cross-sectional single-centre study. BMJ Open 2014;4(4).
- Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res 2010;132:195-200.
- Anandakumar D, Ratnatunga SS, Dayabandara M, et al. Depressive disorder in patients attending the outpatient department of a tertiary care hospital in Colombo. The Ceylon Medical Journal 2016;61(3):118-122.
- Rahman M, Rahman MA, Flora MS, et al. Depression and its association with socio-demographic characteristics among type 2 diabetes mellitus patients of Bangladesh. Mymensingh Med J 2012;21(3):490-496.
- Aujla N, Abrams KR, Davies MJ, et al. The prevalence of depression in white-European and South-Asian people with impaired glucose regulation and screen-detected type 2 diabetes mellitus. PLoS One 2009;4(11):e7755.
- Sridhar G, 12Madhu K, Veena S, et al. Living with diabetes: Indian experience. Diabetes Metab Syndr 2007;1:181-187.
- Shobhana R, Rao PR, Lavanya A, et al. Quality of life and diabetes integration among subjects with Type 2 diabetes. J Assoc Physicians India 2003;51:363-365.
- Gudelj-Radić J, Davidović D, Avramović D, et al. Factors mediating the depression in the adult obese outpatients. Srp Arh Celok Lek 2007;135(1-2):61-66.
- de Groot M, Anderson R, Freedland KE, et al. Association of depression and diabetes complications: a meta-analysis. Psychosom Med 2001;63(4):619-630.
- Arambewela MH, Somasundaram NP, Jayasekara HBPR, et al. Prevalence of depression and associated factors among patients with type 2 diabetes attending the diabetic clinic at a tertiary care hospital in Sri Lanka: A descriptive study. Psychiatry J 2019;2019:7468363.